When an adult has a mental illness, family and friends who care about that person are often told there's nothing they can do to help or, worse, that they are to blame and need to "stay out of it". The science of recovery from mental illness tells a very different story. In fact, strong supportive relationships are among the top predictors of recovery from mental illness, and treatment programs that include and support a patient’s family members have the best outcomes for severe mental illnesses like schizophrenia, schizoaffective disorder and bipolar disorder. Even some programs that include family members only (without the patient) can lead to significant improvements for both the family and the patient.
If you have a loved one with a mental illness, you have a powerful role to play.
Akin Mental Health is here specifically to help you, the family. We want to share with you in this article some of the powerful research that we are using to build our program at Akin.
Let’s start with some definitions so that we’re all on the same page about the important concepts of mental illness, family and recovery.
Let’s start with some definitions so that we’re all on the same page about the important concepts of mental illness, family and recovery.
Mental Illness
Using the term mental illness can be controversial. The reason we use the term “mental illness” here is to recognize that while everyone has mental health (just like everyone has physical health), not everyone has the added challenge of a mental illness. We want to honor the hard work and strength that it takes for individuals with mental illness to overcome those challenges on their path to recovery.
The term illness may also be helpful in the pursuit of more needed attention and funding for proper healthcare to address mental illness (e.g. therapy services, case management, medications, rehabilitation, medical professionals, hospitals). There is an urgent need for more availability and recovery oriented care.
Recognizing mental illness as an illness is also important as a family member because it helps you to not frame mental health challenges as a moral, character or ethical failing. It is so easy to get caught up in blame, shame and guilt within a family affected by a mental illness. Sometimes that looks like blame and shame of the individual experiencing symptoms and sometimes that looks like blame and shame of ourselves.
When someone has a physical injury like a broken leg it’s visible and usually easy to identify the origin. The injuries and symptoms of mental illness are typically invisible, hard to trace or shrouded in secret. We’re prone to make destructive assumptions or internalize stigma. Talking about mental illness as an illness can be a useful tool to create curiosity and foster non-judgmental conversations.
Finally, if the term ‘illness’ is causing difficulty in your family around communicating, then we encourage you to let go of this term. Use the language that is helpful to you to find common ground and a shared narrative.
The research highlighted in this article focuses specifically on mental illnesses that involve psychosis, primarily schizophrenia and schizoaffective disorder as well as some bipolar disorder. These are some of the hardest to treat mental illnesses which makes the research on their recovery that much more powerful.
Family
If you google for a picture of a ‘family’, you’ll see lots of pictures of young children and babies with their parents. But family doesn’t end after childhood. Adult relationships of all kinds, with spouses, friends, parents, cousins, aunts, uncles, etc. are all important family connections. It is these adult, chosen relationships that are the type of family we’re talking about supporting recovery in mental illness, whether by blood or by strength of relationship. Most severe mental illnesses either start or intensify in young adulthood – after the age of 18. Just because the legal system recognizes an adult at age 18 doesn’t make their family relationships less important.
It is a common myth that people with severe mental illness aren’t in contact with any friends/family or don’t want them involved in their treatment. In fact, when researchers reviewed historical records of patients admitted to inpatient psychiatric facilities the staff successfully contacted family or friends 75% of the time. Only 8% of patients refused to have the staff call a family member on their behalf. In a separate study 78% of adult patients with severe mental illness who were in contact with their family indicated that they would like their family to be involved in their mental health care.
Of course, the role of this involvement is important. Being involved in treatment is not the same thing as being in control of treatment. In fact, a core benefit of having family involvement is to advocate clearly for the patient's wishes in treatment to the clinical team and lift up the voice of the patient.
Recovery
In another post, we've written about how recovery from mental illness looks different for everyone. In a nutshell, recovery is living a life of flourishing, while successfully managing any symptoms of mental illness which may or may not persist. Recovery from a mental illness doesn’t require an absence of the illness or an absence of treatment. In fact, using treatment services (for example calling a suicide hotline when having suicidal thoughts) can be an important sign of recovery because it shows an ability to manage symptoms proactively. Life still has many ups and downs. Every human life is a constant work in progress.
People from all walks of life live in recovery from mental illness, but there is still so much stigma surrounding mental illness (particularly psychotic disorders) which makes it hard to find these stories. There are a growing number of first hand accounts of recovery from mental illness including Bethany Yeiser, Elyn Saks, Ellen Forney, Andy Dunn and a collection of others.
What can the research tell us about the connection between mental illness, family and recovery?
There have now been several decades of research on treatments for mental illness. The research in this area has shown a clear link between family dynamics and the outcomes for the person experiencing mental illness. Specifically, family conflict (often resulting from symptoms of the illness) can lead to relapse. On the other hand, supportive family relationships can create steps to recovery. Families who work together to reduce conflict, build mutual respect and solve problems together can create an environment more supportive of recovery. This research shows that the way a family responds to a mental illness in a loved one makes a difference.
When a person’s family is involved in the treatment and recovery process for mental illness there can be truly remarkable results.
Recently, researchers in Germany set out to identify the most effective treatments for schizophrenia (and related disorders) which could be used in addition to medication to reduce relapse (i.e. going back to the hospital). The results of this effort were published in one of the most well respected scientific journals in psychiatry, The Lancet, in October 2021. Bighelli and colleagues gathered all the studies they could find from all over the world that tested what are referred to as ‘psychosocial interventions’ for schizophrenia (in addition to medication prescriptions) and studied follow-up after one year to see which treatments kept the patients from returning to the hospital. Most of the treatments in these research studies focused solely on the patient with mental illness (e.g. CBT therapy, health education, social skills training). A few of the treatments involved the patient's family as well.
Remarkably, of all the types of treatments studied, the so-called ‘family interventions’ – the treatments that had the highest attention paid to the family – were the number one most effective treatments at reducing relapse.
The analysis showed that these treatments reduced relapse at the one year mark by 50% compared to treatment as usual (i.e. just medication). Instead of returning to the hospital within a year 35% of the time, patients treated together with their family in these studies only returned on average 16% of the time at the 1 year mark.
Family treatments
Family treatments involve the family as a critical part of the care team and include support for the family's needs as one of the goals of treatment (which are often different needs than the person experiencing mental illness).
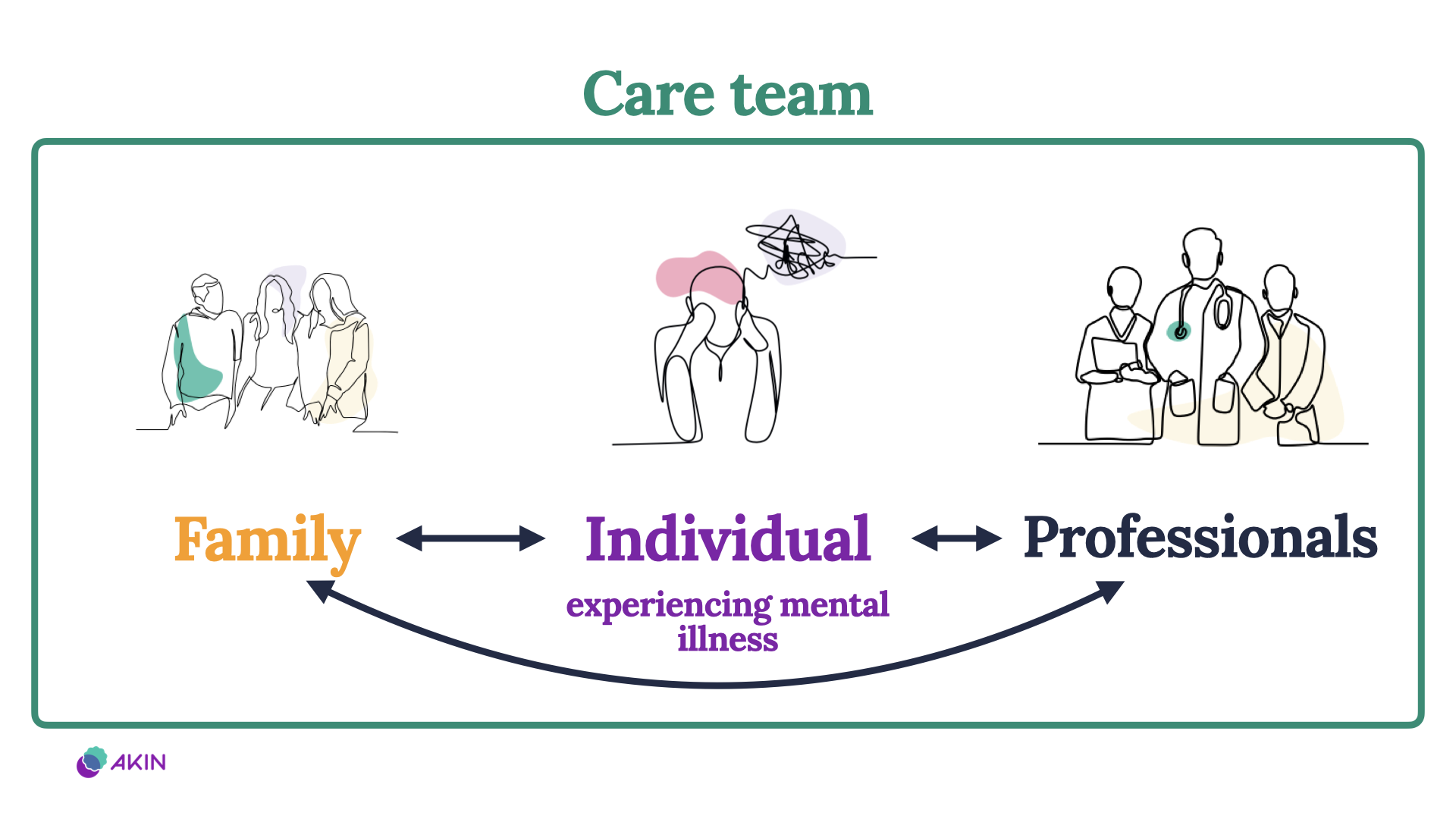
The aims of the family treatments are included in the table below with the language that the researchers used to describe the aims on the left and a summary of that point on the right. The key thing that was different about the family treatments is that they focus on creating an “alliance” – getting everyone on the same team.
If you have a loved one with severe mental illness, you know that it can be very challenging to stay on the same page and on the same team. That’s why having support from a care team for the family as a whole can be so valuable.
| Research description | Summary |
|---|---|
| “Construction of an alliance with relatives who care for the person with schizophrenia” | Get everyone on the same team |
| “Reduction of adverse family atmosphere” | Reduce conflict |
| “Enhancement of the capacity of relatives to anticipate and solve problems” | Improve planning and problem solving |
| “Maintenance of reasonable expectations for patient performance” | Build empathy and understanding |
| “Attainment of desirable change in relatives’ behaviour and belief systems.” | Improve family skills and mindset |
This research clearly shows that when family members are actively engaged as part of the treatment with their loved one with mental illness there is a remarkable benefit. This does take time and hard work from the family members. Families in these treatment programs needed to consult regularly with the care team, get their own education in mental illness and even confront some of their own behaviors and beliefs.
These effects are not because the symptoms are the family's fault but rather because the family's response matters. When families learn to handle the symptoms differently, the symptoms start to respond differently as well. Furthermore, you (the family member) matter too. Family treatments work by helping the family members with their own stress and coping. When family members can get support and stress relief everyone benefits.
Life saving impacts of family involvement
A separate study explored the question of how family involvement in treatment affects outcomes not just one year out but rather an entire decade later. This study included just over 500 individuals with a first episode of psychosis whose families were either fully involved in a program designed for families of the patients or less involved/absent. After 10 years, the patients whose families were fully involved had a 90% reduction in the risk of death from unnatural causes. Not only is family involvement helpful, but this evidence shows that it can be genuinely life saving.
The paradox of family involvement
Imagine running a marathon, pushing as hard as you can at mile 22 sweating hard and not sure if you can make it the last 4 miles. A crowd is gathered along the sidelines to cheer on the racers. But instead of shouting encouraging words like “keep going”, “you can do it”, “you’re awesome” they are instead shouting at you “give up”, “go home”, “the pain isn’t worth it”, “you have no place here”, “there’s no end in sight”. This is something like what supporting a loved one with mental illness can feel like. (Except it’s more like a 100 mile night run through the Rockies and you’ve lost count of the mile markers.)
Our culture, and even the medical treatment system, is designed to isolate people with mental illness rather than encourage connection. The paradox is that isolation and mental illness are really two sides of the same coin. Isolation makes everyone less healthy. While mental illness happens in isolation, mental health happens in relationships. When you stay connected and learn not to let the symptoms of mental illness win over the relationship, everyone can start to heal together.
Akin Mental Health is here to train with you
Going back to the metaphor of running a marathon – if you set out to run a marathon you would want more than a cheering crowd. You’d probably want to talk to others who have done it before, get tips on the best gear/techniques and even work with an experienced trainer. Akin Mental Health is built on this same concept but for the purpose of caring for someone in your life who is experiencing mental illness.
The program at Akin is built from the extensive research (discussed above) on what families need to learn and do to have the best impact on recovery from mental illness. We curate this research with experts and experienced family members to bring it out of the lab and over to you. Live workshops bring together other families experiencing similar challenges to discuss the information and share stories and perspectives. Sometimes the most helpful thing is just to feel the validation of talking to someone else who has been in your shoes.
If someone you love is struggling with a mental illness you might have been focused exclusively on what they are doing (or not doing). We hope that the research discussed here inspires you to think more about what you can learn and do as well. The number one piece of advice we hear from family is to start by focusing on your own support (put on your own oxygen mask first). When you approach mental illness in this way, the results can be remarkable.